Joint Research with SML Biopharm…Anticancer Effects Verified in Animal Models
Published Online in International Journal ‘Advanced Science’
Catholic University announced on the 31st that Professor Nam Jae-hwan’s research team in the Department of Biomedical Sciences has, together with the biotech company SML Biopharm Inc., developed Korea’s first personalized mRNA cancer vaccine (PCV).
The study involved Professor Nam, first author Seongje Jo (PhD candidate), professors Yun Hyun-ho and Kwak Uri of Catholic University, Professor Kim Kwon-il of Kyung Hee University, Professor Kim Ki-tae of Seoul National University, Professor Jang Jun of Ewha Womans University, and the SML Biopharm research team.
Global interest in personalized cancer vaccines for prevention and treatment is increasing. In particular, following the COVID-19 pandemic, the safety and rapid manufacturing capabilities of mRNA vaccine technology have been demonstrated, accelerating the development of “personalized therapeutic vaccines” tailored to individual patients’ tumor characteristics.
U.S. companies BioNTech and Moderna are conducting clinical trials targeting melanoma, lung cancer, and other cancers. Some vaccines have shown meaningful results as adjuvant therapies to prevent recurrence after surgery.
Professor Nam’s team used an mRNA platform to directly manufacture a therapeutic vaccine based on an individual’s tumor genetic information for the first time in Korea, and demonstrated its anticancer efficacy through animal experiments.
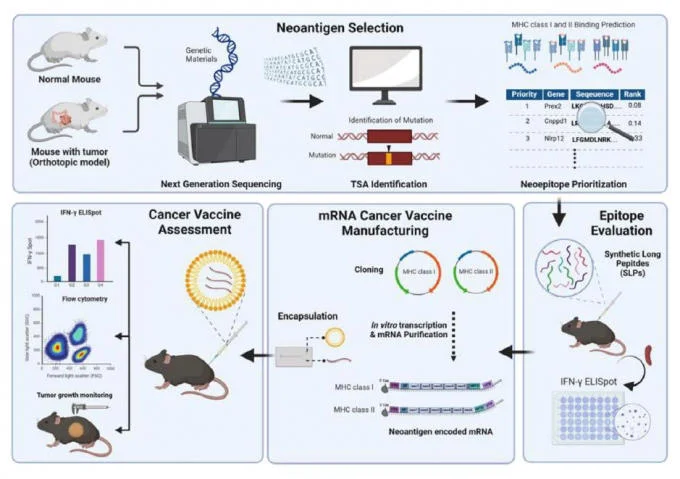
The researchers conducted the study using a mouse model of colorectal cancer. First, they used next-generation sequencing (NGS) to select neoantigens present only in cancer cells, then produced mRNA vaccines encoding those neoantigens, encapsulated them in lipid nanoparticles (LNPs), and administered them by injection.
Experimental results confirmed that tumor-specific immune cells (CD8+ T cells and CD4+ T cells) were activated, leading to tumor growth inhibition, prevention of post-surgical recurrence, and the formation of long-term immune memory.
Notably, neoantigens presented via the MHC-II pathway induced stronger antitumor immune responses than those via the MHC-I pathway, which has been the primary focus of previous studies. When neoantigens from both pathways were administered simultaneously, a synergistic effect enhanced anticancer efficacy, and co-administration with immune checkpoint inhibitors (such as PD-1 and Tim-3 inhibitors) markedly improved outcomes. In addition, postoperative vaccination reduced recurrence rates, and efficacy as a preventive vaccine was also demonstrated in animal models.
Professor Nam said, “This is the first case in Korea in which an mRNA-based personalized cancer vaccine was directly manufactured and its anticancer efficacy verified. The fact that the vaccine can induce long-term memory and maintenance of immune cells capable of directly attacking cancer cells may provide important clues for preventing cancer recurrence and strategies for managing chronic cancer.”
The research was supported by the Ministry of Food and Drug Safety projects “Development of Toxicity Evaluation Technologies for mRNA Vaccines, etc.” and “Establishment of a Safety Assessment Platform for mRNA-based Neoantigen Cancer Vaccines and International Cooperation.” The results were published online in the internationally respected journal Advanced Science.
MoneyToday reporter Kwon Tae-hyeok (https://news.mt.co.kr/mtview.php?no=2025073114051020854)